Friday, April 26, 2019
IMMUNOLOGY OF HIV INFECTIONS part 13
Although the story of the African sex workers who seem to be immune to HIV infection has captured the imagination of many researchers, there is another model of natural immunity that needs examination in more detail. Most babies born to HIV-infected mothers also escape infection even after potential intrauterine exposure and, more important, exposure to virus-containing blood and secretions during labor and delivery. Finally, breast-fed infants ingest hundreds of liters of virus-infected breast milk. Many factors such as CD4 cell counts and viral load in the secretions must be considered. One should add that, like the sex worker model, it is a "real"-world situation of viral encounter opening a window to the "in vivo" infection moment. Although interesting, there are, however, several drawbacks to the model; notably, the newborn is immunologically immature compared with later in life. However, their capacity to produce CC cytokines is greater compared with their mothers whether she is HIV infected or not. This is consistent with the expected skewing toward a stronger innate response rather than the adaptive response.
IMMUNOLOGY OF HIV INFECTIONS part 12
DC interaction with HIV is relevant to the pathogenesis of AIDS because they are present in the mucosa and skin of humans and are believed to be the first HIV-1 targets following sexual transmission of the virus. Both myeloid DC and plasmacytoid DC possess the receptors for HIV entry ; that is, CD4, CXR4, and CCR5 can be infected but with a lower efficacy than CD4 cells or macrophages. The long-term result of this infection is that DC remains a reservoir for the production and persistence of the HIV-1 virus, and the virus induces several functional impairments and variations in the DC populations. Thus, the number of both myeloid DC (MDC) and peripheral DC (PDC) are significantly decreased in HIV-positive progressors, while remaining unaltered in HIV-positive long-term nonprogression. The destruction of these cells may be a consequence of direct lytic infection or as targets for specific CTL or through a block in DC development from peripheral CD34 stem cells. More recent evidence supports the notion that both midi and pad show impaired functional capacity in HIV-positive patients. Since both DC subsets participate in the initiation of innate and adaptive immune responses, infection, depletion, and dysfunction of DCs may contribute to the immunesuppression seen in HIV disease. Therefore, DCs play a dual role in HIV infection: they trigger both innate and adaptic immune responses to control the infection, but they also represent a viral reservoir for infection of permissive CD4 T cells.
IMMUNOLOGY OF HIV INFECTIONS part 11
One of the key cells in the immune surveillance system is the native DC, which is well equipped for activation of both the innate and adaptive immune response. It has been demonstrated that some DC-tropic viruses such as influenza virus leave DC function intact while other viruses such as HIV and cytomegalovirus have evolved strategies to impair DC functions, thereby enhancing the virus's ability to persist and escape immune surveillance.
IMMUNOLOGY OF HIV INFECTIONS part 10
Further studies of these women centered around the known polymorphisms of the IL-4 gene and resistance to infection. Using microsatellite genotyping methods coupled with the genomic sequencing, three polymorphisms in the interferon regulatory factor (IRF-1) located at 619a, 179, and 6516 of the gene, showed association with resistance to HIV infection. Peripheral blood mononuclear cells from these patients showed significantly lower-based IRF-1 expression and reduced responsiveness to IFN-γ stimulation. This study added IRF-1, a transcriptional immunoregulatory gene, to the list of genetic correlates of altered susceptibility to HIV-1.
IMMUNOLOGY OF HIV INFECTIONS part 9
Perhaps more important has been the examination of the CD8 cells in these ESN individuals. Because IFN-γ production correlates with cytotoxic functions, the CD8 T lymphocyte IFN-γ response to HIV p24 peptide in ESN women was compared with HIV-positive individuals. Approximately 40% of ESN women had a CD8 IFN-γpositive response, and this was five times lower in magnitude than that of HIV-positive women. The breadth of the response was very narrow and focused primarily on one peptide that is similar to KK10 protective peptide when compared with the HIV-positive group. In HIV-positive women, lower CD4 counts influenced the number of CD8 cells producing IFN-γ, which may undermine the ability to control HIV. These results indicate ESP women have an HIV-1 p24 peptide-specific CD8 IFN-γ response, providing evidence to the specificity needed for an effective HIV vaccine.
IMMUNOLOGY OF HIV INFECTIONS part 8
Turning first to examinations of CD4 T-cell immune responses in seronegative sex workers compared with HIV-positive women, CD4 T cells that produced interferon gamma (IFN-γ) in response to HIV p24 were detected in exposed seronegative sex worker (ESN) women, albeit at a much lower level than in HIV-positive women. However, ESN women had a 4.5-fold stronger CD4 proliferation response to the p24 peptide compared with the HIV positive group. These data suggest that CD4 T cells in ESN women recognize HIV and have an enhanced ability to proliferate to the p24 protein.
IMMUNOLOGY OF HIV INFECTIONS part 7
Approximately 5-10% of sex workers in Kenya remained HIV uninfected despite engaging in unprotected sex with many male clients and the frequent acquisition of other sexually transmitted infections. Because of the pioneering work of Plummer and associates, the scientific reasons for this extraordinary resistance to the virus in these women are beginning to unfold.
IMMUNOLOGY OF HIV INFECTIONS part 6
In summary, the selective effects of the NEF protein may markedly enhance viral pathogenesis and progression to disease. It does this by hijacking DC functional activity and favoring HIV replication via bystander activation of CD4 cells and the escape of HIV-1 from immune surveillance by blocking NEF influence in viral replication may have long-term beneficial effects on therapeutic management of the disease.
IMMUNOLOGY OF HIV INFECTIONS part 5
More recently, a large body of evidence has appeared that shows that NEF has many important effects of many cells of the immune system. Both exogenous and endogenous NEF down-regulates HLA-ABC molecules critical for the initiation of cytotoxic T lymphocyte (CTL) responses, thus impairing antigen presentation to HIV-specific CD8 lymphocytes. NEF and gp 120 also are able to down-regulate major histocompatibility complex class I (MHC-I) in dendritic cells (DCs) and introduction of exogenous NEF leads to up regulation of MHC-II molecules, thereby favoring CD4 T-cell activation. This step increases the "pool" of lymphocytes permissive to infection. However, endogenous NEF does not modulate MHC-II surface expression; rather it induces a loss of co-stimulation. These results underscore the pleiotrophic action of NEF. On one hand, exogenous NEF triggers ABC-mediated bystander T-cell activation, ensuring viral spread, while endogenous NEF induces a loss of co-stimulation, favoring immune evasion.
IMMUNOLOGY OF HIV INFECTIONS part 4
One of the earliest markers in the progression of HIV-1 infection was the presence of NEF in the viral strain. NEF is a 27-34 D myrisolated protein unique to primate lente viruses. A functional NEF protein is important for the development of high viremia and AIDS in simian immuodeficiency virus (SIV) in infected rhesus macaques. An important observation first noted in the macaques and later in humans was that animals infected with NEF-deleted virus were resistant to subsequent challenge with pathogenic wild-type viruses. This was followed by the observation in humans that some individuals with long-term non-progressive HIV-1 infection (persons who showed no clinical or immunological signs of immunodeficiency despite being HIV seropositive for over a decade) turn out to be infected with viruses carrying deletion in their NEF gene.
Tuesday, April 23, 2019
IMMUNOLOGY OF HIV INFECTIONS part 3
IMMUNOLOGICAL AND BIOLOGICAL PARAMETERS OF DISEASE
The pattern of disease progression has now been well documented. Following infection with the virus, the virus hones to and infects cells with CD4 receptors. During the early phase, individuals may experience a flu-like illness with mild fever, cough and occasional chills. The symptoms subside, and the individual may be asymptomatic for many years. In realty, the disease is progressing, and it is a long battle between the immune response with production new CD4 cells and the dying (apoptotic) HIV-infected CD4 cells. Eventually, the host immune system deteriorates, and the individual succumbs to the complications secondary to loss of the cellular immune system. The pattern and complications are quite similar to those seen in primary immunodeficiency diseases. However, it has been a well-known observations that some individuals, especially sex workers with repeated exposure to the virus, are relatively resistant to HIV acquisition.
IMMUNOLOGY OF HIV INFECTIONS part 2
Thus, many researchers are focusing on studies of the immunological concepts involved in the disease, not only to understand in greater detail why some individuals remain uninfected (they are not immune since some "resistant" women later acquire human immunodeficiency virus, HIV), despite repeated exposure to infected individuals, but also to explore various vaccine candidates and concepts that might prevent the disease before exposure to the virus-candidates that would be cheap to make and inexpensive to deliver.
IMMUNOLOGY OF HIV INFECTIONS part 1
An estimated 33 million people globally are infected with the AIDS virus (HIV-1). Most of the infected individuals are poor, live in developing countries, and have little access to health care. Although initiatives are under way to bring proper medications to these individuals via a large infusion of money, this will only approximately 2.5 million individuals and prevent 12 million new cases, as pointed out in a 2007 New York Times editorial. The remainder of these infected individuals will continue to increase the number of newly infected individuals. In this context, the medications decrease the viral load in treated individuals, but medications are expensive and would not reach many of the infected individuals living in developing countries.
CHRONIC LYMPHOCYTIC LEUKEMIA part 32
New knowledge about the biology of B-CLL can provide clues for novel therapeutic targets. For example, since B-CLL cells must interact with the stroma in bone marrow or other peripheral lymphoid tissues to survive, furthering our knowledge of these interactions may generate new objectives for innovative therapies. Another compelling set of options may derive from specific inhibition of the BCR or CD38 signalling pathways or other pathways in which ZAP-70 is crucial. Likewise, the possibility of using cell-cycle-specific drugs is worth being explored in clinical trials, given the documented active turnover of B-CLL cells. Finally, because up to 20% of patients with the worst prognostic markers have stereotypic antigen receptors, these common structures may be feasible as vulnerable points of attack. As the antigens that engage these receptors become more precisely defined, it may be possible to use these to develop an arsenal of specific therapies.
CHRONIC LYMPHOCYTIC LEUKEMIA part 31
The new prognostic markers indicate that 30-50% of the patients have features portending a poor outcome, and therefore an early start of therapy may be justified in such poor-prognosis groups. This strategy is plausible, considering that continued proliferation and expansion of the neoplastic clone fascilitates accumulation of ominous cytogenetic abnormalities. However, before any recommended guidelines can be proposed, clinical trials must test the use of early intervention in patients in poor prognosis groups.
CHRONIC LYMPHOCYTIC LEUKEMIA part 30
CLINICAL IMPLICATIONS AND THE DEVELOPMENT OF NOVEL THERAPEUTICS
Currently used clinical staging systems defined by Binet help clinicians to monitor disease progression and decide when to treat patients. Because of difficulties distinguishing patients with poor prognosis at the onset of disease using these staging systems, the generally used practice is to wait to start therapy until the patient's clinical course becomes evident ("wait and watch" mode). However, the molecular and cellular markers that reflect intrinsic properties of leukemic cells present at the disease onset can help to distinguish patients that will follow worse clinical courses, regardless of the Rai and Binet categories at diagnosis. Although determination of IgVH gene mutation status is not yet routinely available, measurement of CD38 and ZAP-70 has become more widely available. Thus, although the wait-and-watch mode is still being followed in current clinical practice, it may substituted for by new more aggressive strategies in the future.
CHRONIC LYMPHOCYTIC LEUKEMIA part 29
Finally, transfer of human B-CLL cells into immune-deficient mice may bypass the ex vivo apoptosis tendency of B-CLL cells, enabling their survival and amplification in vivo. Such an approach may also make it possible to define and test new therapeutics to treat this currently incurable disorders.
CHRONIC LYMPHOCYTIC LEUKEMIA part 28
In the third tramsgenic model, overexpression of APRIL (a proliferation inducing ligand ) in murine T cells leads indirectly to B-cell proliferation and survival because of signaling through its receptors BCMA and TACI. Unlike the previous two transgenic animals, however, expansion of CD5 B cells occur in only 40% of animals, with these B cells locating predominantly in the spleen and rarely passing into the blood. Nevertheless, as APRIL's action involves the TRAFs and leads to NFκB activation, this model may prove helpful in linking signals from soluble ligands and surface receptors to the NFκB pathway, a pathway known to be constitutively active in some B-CLL clones.
CHRONIC LYMPHOCYTIC LEUKEMIA part 27
Another mouse model that develops features resembling human B-CLL involves the overexpression of two genes: BCL-2 and TRAFT2 (TNF-receptor-associated factor 2). This double transgenic animal is especially intriguing because of the already mentioned recent work showing that the deletion at 13q14, often see in human B-CLL, involves the loss of micro-RNAs 15a and 16-1, which affects expression of BCL2. As with the TCL1 transgenic mice, these animals develop CD5 B-cell clones, eventually with massive splenomegaly and leukemia.
CHRONIC LYMPHOCYTIC LEUKEMIA part 26
Transgenic mice expressing the TCL1 gene in murine B cells develop a polyclonal expression of B lymphocytes early in life that becomes progressively more restricted until a monoclonal population emerges after about one year in most animals. The genetic and phenotypic features of this murine leukemia resemble those of the aggressive, treatment-resistant cases of human U-CLL. Although it is of interest that TCL1 is an activator of the P13K-Akt oncogenic signaling pathway, a pathway not infrequently active in human CLL, the extent to which overexpression of this gene leads to human B-CLL remain to be elucidated, as an over expression of TCL1 in human B-CLL patients is not uniform.
CHRONIC LYMPHOCYTIC LEUKEMIA part 25
In recent years, however, a variety of transgenic mouse models have been developed that lead to diseased phenotypes resembling human B-CLL more closely and reproducibly. We focus on three models that have been especially helpful.
CHRONIC LYMPHOCYTIC LEUKEMIA part 24
ANIMAL MODELS OF B-CLL
While an enormous amount of new information has been gleaned by directly studying human B-CLL cells, animal models are now contributing to our understanding of the human disease. For example, New Zealand Black (NZB) mice spontaneously develop, with age, an expansion of IgMCD5 B cells that resembles B-CLL. However, because frank leukemia occurs randomly in only a minor subset of animals, this model has been used sparingly.
CHRONIC LYMPHOCYTIC LEUKEMIA part 23
Because in vitro observations demonstrate the absence of lesions in the major apoptotic pathways, the model posits the absence of an intrinsic cell death defect in the majority of the leukemic clones. We do not rule out the possibility that developing genetic alterations in the evolving clone can tip the balance between pro- and anti- apoptotic molecules in such a way as to favor B-CLL cell survival. However, the influence of external signals appears to dominate based on current knowledge. This is in line with the in vivo labeling studies indicating the dynamic nature off CLL clones.
CHRONIC LYMPHOCYTIC LEUKEMIA part 22
SUMMARY REMARKS ON THE DEVELOPMENT, GROWTH, AND EVOLUTION OF B-CLL
On the basis of the foregoing information, we propose a model for the development of B-CLL. B-CLL cells are able to avoid apoptosis and even to proliferate by receiving growth and stimulatory signals from the environment delivered through their BCR or other receptors; these signals likely involve autologous and foreign antigens, cytokines, and chemokines, as well as yet-to-be-defined ligand on accessory and stromal cells. The cell's BCR mediates major growth effects in cases for which the receptor is polyreactive, binding autoantigens and foreign antigens, while maintaining its capacity to transmit stimulatory signals to the cell nucleus. Both self-reactivity and intact BCR signal-transducing capacity are more frequently found in U-CLL;hence, the more active clonal expansion and clinical aggressiveness of patients with such clones.
CHRONIC LYMPHOCYTIC LEUKEMIA part 21
These considerations are in line with the results of in vivo labeling experiments that involve incorporation of nonradioactive deterium into newly synthesized DNA of dividing cells. These studies have shown B-CLL clones to be dynamic, having measurable birth rates from about 0.1 to>1.0 percent of the clone/day. Although only a minority of cells in a B-CLL clone can be shown to divide using this approach, estimates of the leukemic cell burden of typical B-CLL patients are of the order of about 10(12) cells, and therefore about 10(9) to 10(10) new leukemic cells would be generated daily. Such rates of cell division are sufficient to permit more dangerous clonal variants to emerge and to influence clinical course and outcome over time.
CHRONIC LYMPHOCYTIC LEUKEMIA part 20
Similarly, there is a rough correspendence between the clinical course of patients and the development of chromosomal abnormalities in their clones. Recurrent chromosomal lesions typically found in B-CLL patients include deletion at 13q14.3,11q22-23,17p13, and 6q21, and amplifications of all or portions of chromosome 12. Deletion at 13q14.3 is found in greater than half of B-CLL cases over time and is linked to loss of two micro-RNAs that can regulate Bcl-2 expression. However, thus particular chromosomal abnormality is not especially dangerous because patients exhibiting this deletion on one allele and no other DNA lesions in their clones have a clinical course that is benign and comparable to normal age-stratified individuals. In contrast, deletions at 11q22-23, 17p13, and 6q21 are generally associated with more aggressive disease, perhaps because these deletions may affect important genes such as p53 (17p13 deletion), and ataxia telangiectasia mutated (ATM; 11q22-23 deletion). Longitudinal studies, albeit on a relatively limited number of patients, demonstrated that these ominuous cytogenetic abnormalities accumulate progressively in the course of the disease and more frequently in patients with U-CLL.
CHRONIC LYMPHOCYTIC LEUKEMIA part 19
CORRELATIONS BETWEEN THE CELLULAR AND MOLECULAR FEATURES OF THE DISEASE WITH THE CLINICAL COURSE OF B-CLL
How might features of the repertoire of IgVH genes used by B cells in B-CLL, the mutations status of these genes, and expression of molecules related to cellular activation and BCR signal transduction (CD38 and ZAP-70) be relevant to the clinical course of B-CLL? These disease manifests differently in different patients, depending on the utilization of mutated or unmutated IgVH genes and the expression of ZAP-70 and CD38 by the leukemic cells. One explanation is that activation via the BCR following recognition of (self) antigens activates the cells in vivo, accompanied by expression of CD38 and ZAP-70. Because the majority of U-CLL clones contain a self-reacting BCR, while most M-CLL clones do not, it is not unexpected that more activation markers are found on U-CLL cells. In addition, B-CLL clones from patients in different prognostics subsets differ in signaling capacity, with an intact BCR signal transductions pathway found most frequently among patients exhibiting unfavorable prognostic markers. Thus, continuous (auto)antigenic stimulation would likely represent a major factor for U-CLL cases and much less likely for M-CLL.
CHRONIC LYMPHOCYTIC LEUKEMIA part 18
In addition to antigen stimulation, B-CLL cells also receive receptor-mediated signals as well as soluble factors, such as cytokines and chemokines, from other lymphoid and nonlymphoid cells. In particular, it is thought that in vivo B-CLL cell interactions with stromal cells and "nurselike" cells can rescue normally (ex vivo) apoptosis-prone B-CLL cells from death. The natural ligand of CD38, CD31, is displayed on stromal and nurselike cells as well as on endothelial cells and might be involved in setting up these rescue signals. Such contact derived and soluble signals can go on to up-regulate anti-apoptotic genes, such as Bcl-2, survivin, and Mcl-1, which could rescue B-CLL cells from apoptosis and fascilitate their growth.
CHRONIC LYMPHOCYTIC LEUKEMIA part 17
A hypothesis such as this implies that it might be possible to detect clonal expansions in healthy subjects. In fact, small numbers of apparently clonal B cells with B-CLL cell characteristics do exist in the blood of about 3.5% of disease-free individuals. An even higher proportion of such clones have been found in the blood of first-degree relatives of patients with B-CLL (as often as 12%). Although such studies of the BCRs of B lymphocyte expansions in normal disease-free individuals are limited, they further support this hypothesis in that these expansions are not only monoclonal but also use some of the same genes commonly encoding the BCRs of B-CLL clones.
Sunday, April 14, 2019
CHRONIC LYMPHOCYTIC LEUKEMIA part 16
With continued expansion leading (or not) to accumulation of IgVH gene mutations as explained by the T-cell-dependent versus T-cell-independent models mentioned earlier, it becomes increasingly likely that a cell develops a genetic abnormality as in an initial inducing lesion that would lead to relatively unrestrained expansion. Such a cell is primed for leukemic transformations.
CHRONIC LYMPHOCYTIC LEUKEMIA part 15
Similarly, such a mechanism could also promote the origin of M-CLL. As already mentioned, IgVH gene mutations can occur without T-cell help in marginal zones outside of GCs. Because mutations can sometimes favor autoreactivity, such autoreactive B cells would become expanded. However, expansion would stop if IgV gene mutations alter BCR structure in such a way that antigen binding is no longer sufficient to induce B-cell signalling.
CHRONIC LYMPHOCYTIC LEUKEMIA part 14
How would the transition from normal B cells to leukemic cells via antigen stimulation occur? Normal B lymphocytes using unmutated IgV genes produce antibodies that are frequently polyreactive, binding carbohydrates, nucleic acids and phospholipids. Such antibodies provide the first line of defense against microorganisms and promote the clearance of autoantigens and their fragments. B-CLL cells frequently display polyreactive BCRs, thereby making it possible that they derive from normal polyreactive B lymphocytes that have been repeatedly stimulated in vivo by a combination of nonprotein self and microbial antigens.
CHRONIC LYMPHOCYTIC LEUKEMIA part 13
Foreign antigens or autoantigens could prompt normal B lymphocytes to become B-CLL cells by selecting B-cell clones with restricted BCRs (possibly unique to B-CLL) is largely unknown, although currently under investigations. It may be they result from infections due to a specific microbe common among patients, which has been found for gastric lymphomas. Alternative possibilities are that both environtmental and autologous antigens may be involved. Indeed, it appears that intermitten and interchangeable encounters with microbial antigens and autoantigens, especially those generated during cell death and oxidative and other forms of stress, are key.
CHRONIC LYMPHOCYTIC LEUKEMIA part 12
In contrast, several stimulatory signals delivered from the microenvirontment may represent important promoting factors in the development and evolution of the disease. One of these - antigen stimulation - appears to play a major role in the pathogenesis of B-CLL; this conclusion is based on the existence of remarkable similarities in the structures of BCRs of unrelated patients. This similarity in BCR structure is especially striking for about 25% of patients, with some patients clones using identical IgVH, D and JH genes. Extraordinarily, in some of these cases, these rearranged Ig heavy-chain genes are paired with identical IgVL genes, yielding antigen-binding sites that are virtually identical at the amino acid level. Given the enormous number of possible combinations of IgV gene segments encoding antibody-binding domains, one would not expect to find B-CLL patients having such structurally similar "stereotypic" BCRs by chance until well over 1 million cases have been screened. Hence, their occurence is not likely random, making a plausible argument for the importance of antigen stimulation and drive in this disease.
CHRONIC LYMPHOCYTIC LEUKEMIA part 11
Despite active research, to date no genetic aberration (inducing factor), shared by all patients, has been found in B-CLL. The monoclonality of B lymphocytes that develop in this disease implies that such a lesion existed in the cells initiating the clone. Although characteristic DNA abnormalities can occur later in the development of B-CLL clones, these are rarely found in the initial phases of the disease.
CHRONIC LYMPHOCYTIC LEUKEMIA part 10
DEVELOPMENT OF B-CELL FROM NORMAL B LYMPHOCYTES:
SIGNALS AND MECHANISMS INITIATING THE GROWTH AND ACCUMULATION OF LEUKEMIC LYMPHOCYTES
The major events in tumorigenesis have traditionally been grouped into inducing and promoting factors. Inducing factors cause transforming mutations, whereas promoting factors sustain the proliferation and survival of cells undergoing or having undergone transforming mutations. It is useful to apply such principles to B-CLL.
CHRONIC LYMPHOCYTIC LEUKEMIA part 9
It is interesting to note the correlation between the molecular characterizations of the patients "clones with the patients" clinical course. Of major clinical and investigative importance are the observations that IgVH gene mutations status and ZAP-70 and CD38 expression have clinical relevance, since cases in whom the majority of the cells express CD38, ZAP-70 and exhibit unmutated IgVH genes have a more aggressive clinical course. Correspondingly, those patients whose clones are in the main CD38 ZAP-70 and express mutated IgVH genes generally fare better and have a good prognosis. In those individual cases that are discordant for the expression of these markers, there is nevertheless generally a direct correlation between the number of unfavorable markers and clinical outcome.
CHRONIC LYMPHOCYTIC LEUKEMIA part 8
In comparing these two subsetting schemes-the first based on IgVH mutation status and the second on activation markers - CD38 ZAP-70 B-CLL clones generally use unmutated IgVH genes, whereas CD38 ZAO-70 B-CLL clones mainly use mutated IgVH region genes. Although the subdivision into CD38 ZAP-70 U-CLL and CD38 ZAP-70 M-CLL is true for the majority patients, it is not universal since about 25% of cases are discordant for the expression of the three markers.
CHRONIC LYMPHOCYTIC LEUKEMIA part 7
B-CLL clones can be further subdivided based on their activation marker expression: in one group, the majority of leukemic cells express two activation markers, that is, CD38 and ZAP-70; and in the other, the majority of the cells lack by the these markers. The two molecules appear to be involved in the regulation of signals delivered by the BCR. The CD38ZAP-70 B-CLL subset is primarily characterized by the presence of more members of the leucemic clone-bearing markers of activated B cells. These activation marker-defined subgroups also differ in their expression of several other molecules up-regulated by cellular activation.
CHRONIC LYMPHOCYTIC LEUKEMIA part 6
B-CLL cells are monoclonal B-cell expansions as documented by the expression of monotypic (ie, either κ or λ) surface Ig and the CD19 antigen; this is in line with the presence of monoclonal rearrangement of VDJ genes in the leukemic cells. Most B-CLL cells also express activation markers and, like normal activated B-cells, have low levels of surface IgM and IgD. The expression of CD5, usually thought of as a lineage marker, is characteristic of B-CLL cells and should be considered part of their activation varies in different B-CLL cases.
CHRONIC LYMPHOCYTIC LEUKEMIA part 5
CHARACTERIZING THE HETEROGENEITY OF B-CLL BY MOLECULAR AND CLINICAL SUBTYPES
Based on their mutation status, B-CLL patients can be divided into two groups those whose B-CLL cells use unmutated IgVHgenes (U-CLL) and those B_CLL cells use mutated IgVH genes (M-CLL). Initially, it was believed that the two types of B-CLL cells could be generated by vigin and memory cells, rsepectively, although, as we shall discuss there is now evidence that both B-CLL subtypes derive from (auto) antigen -experienced B cells.
CHRONIC LYMPHOCYTIC LEUKEMIA part 4
B-CELL ACTIVATION AND MATURATION
The enormous diversity of the normal B-cell-antibody repertoire initiates in the bone marrow where B-lymphocytes rearrange their immunoglobulin (Ig) variable (V) region gene segments coding for the B cell's receptor for antigen (BCR). The diversity in the repertoire continuous to grow after binding antigen, when the B cells enter a lymphoid follicle and, with the help of other cells and cytokines, creates a structure called the germinal center (GC) where the cell proliferates and accumulates somatic mutations in its BCR-encoding genes. These mutations may produce amino acid changes in the binding site BCR, which can improve or create new antigen-binding specificity. Enhanced affinity B cells survive, whereas those having BCRs that either do not bind antigen or bind self-antigens die.The GC reaction usually occurs in secondary lymphoid follicles with the help of T lymphocytes. This mutation and selection process can take place in response to bacteria without T-cell help in the marginal zones outside of lymphoid follicles, although in this case, antigenic stimulation does not always induce mutation of IgVH genes.
CHRONIC LYMPHOCYTIC LEUKEMIA part 3
An abundance of new information has become available within the past decade, such that B-CLL is now divided into two related conditions, both originating from antigen-selected B lymphocytes but differing in clinical course. Some patients lives several decades, often without treatment, and others succumb to the disease in a few years. Here we shall discuss the possible mechanisms causing expansion and conversion of normal B lymphocytes to leukemic clones and determining the differences between the two major B-CLL subtypes. First, we will review B-cell development and the aberrant transformation to leukemia.
CHRONIC LYMPHOCYTIC LEUKEMIA part 2
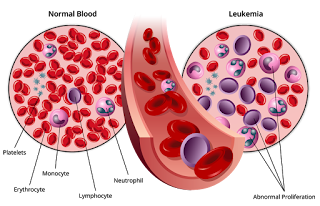
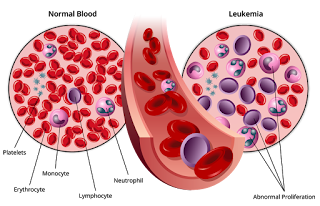
Any cell of the immune system can undergo malignant transformation giving rise to leukemia, lymphoma, or myeloma. We focus on B-cell-type chronic lymphocytic leukemia (B-CLL), the most common leukemia in the Western Hemisphere. This B-cell lymphoproliferative disorder arises among the aging population, increasing in incidence in a linear fashion after age 50. Therefore, its incidence is likely to increase as the baby boomer generation enters the sixth decade. Because patients with the disease in general have an extended clinical course (three to twenty-five years), B-CLL is categorized as one of a group of indolent leukemias/lymphomas. However, despite progress in therapeutic strategies, B-CLL remains an incurable disease.
Wednesday, April 10, 2019
AUTOIMMUNITY part 84
HUMAN EMBRYONIC STEM CELLS
Very recent advances in stem cell technology enable the generation of pluripotent human stem cells using a process known as reprogramming or dedifferentiation. The procedure exploits viral vector-mediated expression of only four genes (namely, c-myc, oct3/4, sox2 and klf4) to program mouse and human somatic cells (specifically, skin fibroblast) into embryonic-like "induced pluripotent stem cells" (iPS cells). These cells appear to be just as plastic as embryonic stem cells, but one draw back to their clinical application in humans is the use of lentiviral or other retroviral vectors to introduce the genes. Although still at an early stage, the use of iPS cells could greatly advance the practicality of regenerative medicine as a therapeutic option. By creating patient-specific, pluripotent human stem cells, cell replacement therapies that avoid human embryo destruction may now be within reach.
AUTOIMMUNITY part 83
Current tissue engineering strategies tend to rely on the use of autologous sources of adult stem cells. However, data demonstrating that the transplantation of allogeneic adult mesenchymal stem cells is feasible have the potential to revolutionize this field. With routine access to adult stem cells at the point of care, physician may be able to incorporate tissue engineering approaches into the management of autoimmune disease.
AUTOIMMUNITY part 82
Interestingly, allogeneic bone marrow-derived MSCs or stromal cells suppress in vitro T- and B-cell proliferation in a non-MHC-dependent manner. The immunosuppressive activity of MSCs has been attributed to effects on the expansion of the CD25CD4Foxp3Treg population
AUTOIMMUNITY part 81
Another advantage is that MSCs can take up and retain introduced genes, a property that can be exploited for the delivery of clinically beneficial proteins to targeted locations. MSCs are also amenable to cryo-preservation, allowing their future use in "off-the-shelf" therapies. Animal studies seeking to reconstitute or repair damaged cartilage, bone, muscle, heart muscle and tendon using MSCs have shown great promise raising the possibility that they might one day be used for repairing tissue damaged by autoimmune attack. Indeed, cell therapy using MSCs can prevent damage to the joints in collagen-induced arthritis and also can ameliorate end-organ damage in EAE and murine lupus.
Subscribe to:
Posts (Atom)